Did you know that February is Age-Related Macular Degeneration (ARMD) month? Here is a break down of the basics of the condition to help you review for clinic, rotations, or boards.
 ARMD is a retinal condition that results in reduced central visual acuity, and ultimately, central blindness. It affects 11 million Americans, and unfortunately, that number is growing. As the name implies, ARMD is a condition typically associated with aging, most commonly found in people 55 years old and up. There are two main forms of ARMD – colloquially known as “wet” and “dry.” Unfortunately, the pathophysiology for both forms remains unclear and there is no cure for either subtype. However, the clinical signs and symptoms allow for differentiation, which grants us the opportunity for the unique treatment/management of each subtype.
ARMD is a retinal condition that results in reduced central visual acuity, and ultimately, central blindness. It affects 11 million Americans, and unfortunately, that number is growing. As the name implies, ARMD is a condition typically associated with aging, most commonly found in people 55 years old and up. There are two main forms of ARMD – colloquially known as “wet” and “dry.” Unfortunately, the pathophysiology for both forms remains unclear and there is no cure for either subtype. However, the clinical signs and symptoms allow for differentiation, which grants us the opportunity for the unique treatment/management of each subtype.
Risk factors for the development of ARMD:
- Age (obviously): Both the presence of the disease and severity increases with age (2% of patients >75 years old… which is a 20x increase compared to patients <55 years old!).
- Smoking: This is the big one – smoking is the largest modifiable risk factor. Patients who smoke tobacco products have shown to be 2-3x more likely to develop Wet ARMD.
- Genetics: There seems to be a genetic component, but the jury is still out on just how much influence a person’s genetic make-up plays in the development of ARMD.
- High fat intake: Trans fats, saturated fats, and omega-6 fatty acids seem to be associated with an increased risk of ARMD (watch out, those on keto-diets!). Monounsaturated fats or omega-3 fatty acids, however, may offer a positive prognosis.
- Race: There also seems to be a slight predilection towards individuals with low amounts of pigment – think blonde hair and blue eyes.
- Additional risk factors include female gender, UV exposure, moderate to severe hypertension, high cholesterol, and increased BMI.
Dry ARMD:
- Accounts for 80% of all ARMD diagnoses, but only 20% of all ARMD legal blindness.
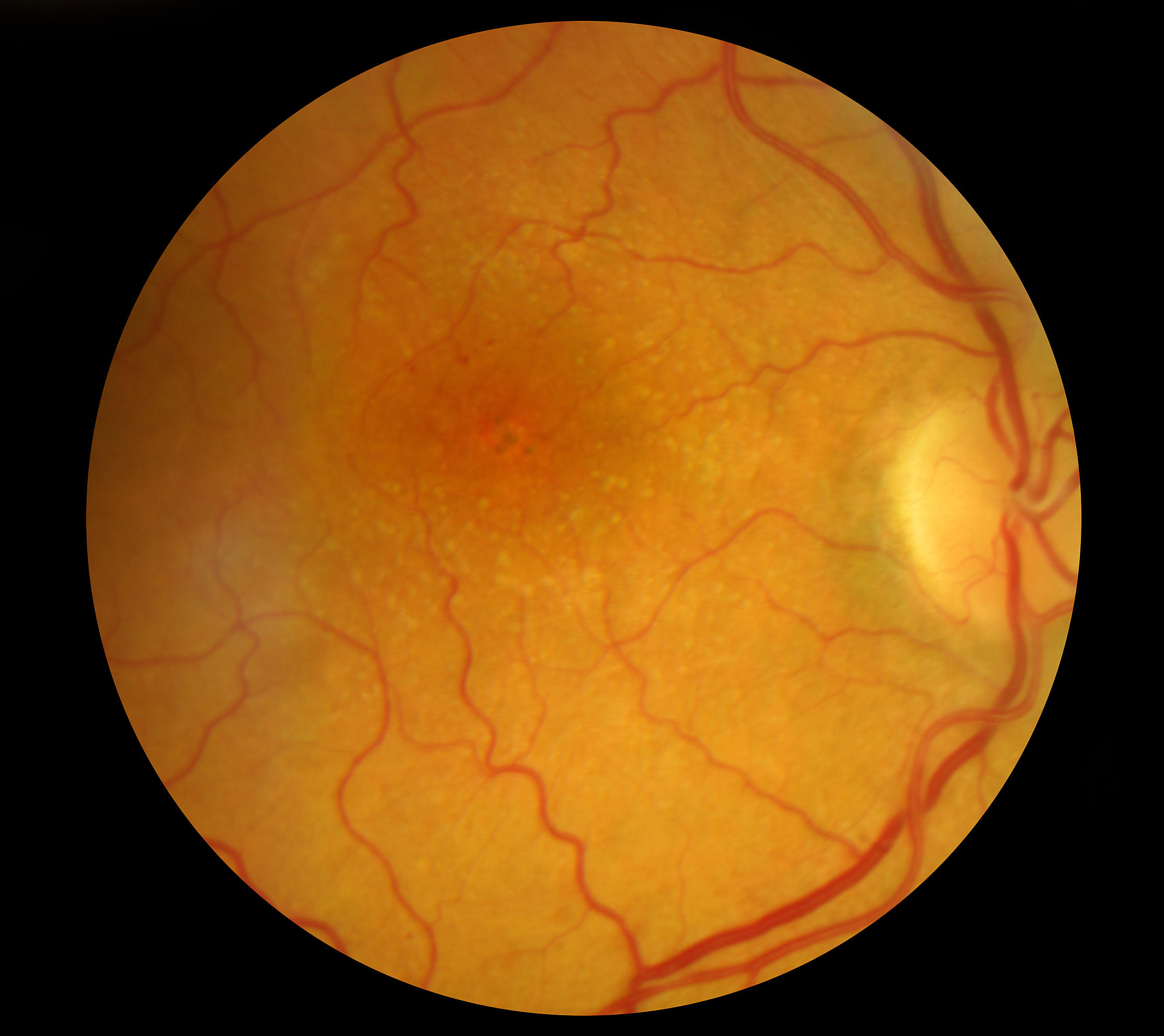
- Characterized by formation of drusen between the choroid and retina. Drusen are fatty acid deposits due to the eye’s inability to clear the photoreceptors’ waste products. In ARMD, those waste products can build-up and create separations/alterations in the sensory retina causing visual distortions called “metamorphopsia.”
- Generally bilateral.
- Can progress to Wet ARMD.
- No medical or surgical treatment currently available.
- Patients’ visual acuity usually ranges from 20/50-20/200, depending on the severity of the disease.
Despite there being no treatment for dry ARMD, according to the AREDS study, there is a vitamin regimen consisting of vitamin C, vitamin E, zinc, copper, and beta-carotene that can slow the progression of moderate dry ARMD to severe dry ARMD (or slow the progression of severe dry ARMD). However, the beta-carotene dosage was linked to an increase in lung cancer for previous/current smokers. Hence, a second formulation was released after the AREDS2 study was conducted in 2006, which marked the removal of beta-carotene, and the addition of omega-3 fatty acids, and the antioxidants lutein and zeaxanthin. The original AREDS formula has been shown to be slightly more efficacious in preventing the progression of ARMD, but AREDS2 is used more commonly due to near-equal efficacy and less risk of lung cancer. For more information, check out our article summarizing AREDS 1 vs AREDS 2.
Patient education is essential in managing ARMD. Educate your patients on their condition and the importance of follow ups to monitor their progression. The goal is to prevent progression to wet ARMD, and the best prognosis is when ARMD is caught early. Encourage patients to quit smoking, wear sunglasses to protect their eyes from UV light, have balanced diets, and monitor their vision with home Amsler grids.
Wet ARMD:
- Accounts for only 20% of all ARMD diagnoses, but 80% of all ARMD legal blindness.
- Characterized by choroidal neovascularization of the retina and blood leakage (hence, “wet”).
- Blood is toxic to the retina – it can cause exudates and even retinal scarring (among other things).
- Typically unilateral onset.
- Can be treated with laser or anti-VEGF intravitreal injections.
- Patients’ visual acuity usually ranges from 20/200-20/800, depending on the severity of the disease (much worse than dry ARMD!)
The neovascularization of the retina from the choroid is due to an upregulation of VEGF signaling in the retina. For this reason, anti-VEGF intravitreal injections are considered the gold standard of wet ARMD treatment. Lucentis (ranibizumab), for example, prevented further vision loss in 95% of patients, showed an improvement in visual acuity by three Snellen acuity lines in 40% of patients, and 40% of patients were able to read the 20/40 visual acuity line or better in its Phase III clinical trials. Other commonly used anti-VEGF drugs include Avastin (bevacizumab) and Eylea (aflibercept), all of which show marked improvement in eyes with wet ARMD.
Age-Related Macular Degeneration is a sight-threatening condition affecting upwards of 11 million people in the United States. Fortunately, we now have fairly effective treatments for wet ARMD. It’s important to be aware of the risk factors and clinical signs/symptoms so this condition can be diagnosed as early as possible, minimizing visual deterioration.
January was glaucoma awareness month – check out our article on how to read perimetry!

