Retroillumination
Retroillumination from the fundus is a quick and easy way to examine the lens, iris, and cornea. The red reflex, the reflection of light off the back of the eye, can be used to highlight opacities in the cornea or lens, and defects in the iris. This article will outline the technique, offer some tricks of the trade, and provide insight into its clinical relevance.
- Procedure Tips
In dim room illumination, adjust the slit-lamp beam width to that of a parallelepiped. Then, shorten the beam height to fit within the pupil to limit light reflecting off the iris (1). Finally, focus the microscope directly on the structure of interest using 10X to 16X magnification. Corneal and lens opacities are best viewed when the patient’s pupils are dilated. When assessing the patency of peripheral iridotomies and iridectomies, a great tip that I learned is to have the patient look down towards your chin, elevate the upper lid, and look for iris transillumination near the 11 and/or 1 o’clock position, where transilluminations are most commonly located.
- Clinical Usefulness
Retroillumination is a valuable tool for assessing corneal dystrophies (e.g. ABMD, Meesmann, Lattice), edema, scars, and vascularization (e.g. corneal pannus, limbal stem cell deficiency) (2). Cortical and posterior subcapsular cataracts are best highlighted against the red reflex. The location and pattern of iris transillumination defects (TID) can help determine the underlying cause.
- Common types of iris transillumination defects and their associations include:
- Pupillary margin: Pseudoexfoliation syndrome –
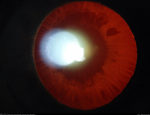
commonly described as a “moth-eaten” pattern near the pupillary ruff. Also look for PXF material on the anterior lens capsule. (Figure 1). - Midperipheral: Pigment dispersion syndrome – commonly in a “slit-like” configuration, most prominent inferiorly or inferonasally. A Scheie stripe (pigment on lens zonules) can also be visualized with retroillumination by having the patient look in different gazes (Figure 2.)

Figure 2 - Diffuse: Albinism, previous acute angle closure glaucoma, Fuch’s heterochromic iridocyclitis, bilateral acute iris transillumination, trauma, and senile iris atrophy.
- Sectoral: Herpes zoster iritis or iris prolapse during phacoemulsification
- Peripheral: Location of iridotomies/iridectomies for angle-closure glaucoma and phakic IOL. Location of toric markers when assessing alignment of toric IOLs.
References
1. Gilman, J.P. (2018, October 20). Slit Lamp Biomicrography Introduction. Retrieved from https://www.opsweb.org/page/slitbiomicrography#
2. Martin, R. (2018). Cornea and anterior eye assessment with slit lamp biomicroscopy, specular microscopy, confocal microscopy, and ultrasound biomicroscopy. Indian Journal of Ophthalmology, 66(2), 195–201. http://doi.org/10.4103/ijo.IJO_649_17.
3. Figure 1. This image was originally published in the Retina Image Bank. Jason S. Calhoun. Pseudoexfoliation Syndrome. Retina Image Bank. 2015; Image Number 25734. © the American Society of Retina Specialists.
4. Figure 2. This image was originally published in the Retina Image Bank. Jason S. Calhoun. Pigmentary Glaucoma, Zonules Visible Inferiorly. Retina Image Bank. 2013; Image Number 7391. © the American Society of Retina Specialists.


