Ptroublesome Ptosis
That ptroublesome ptosis: A patient presents with a new “droopy” lid. So, brilliant optometrist: What are you going to do about it?
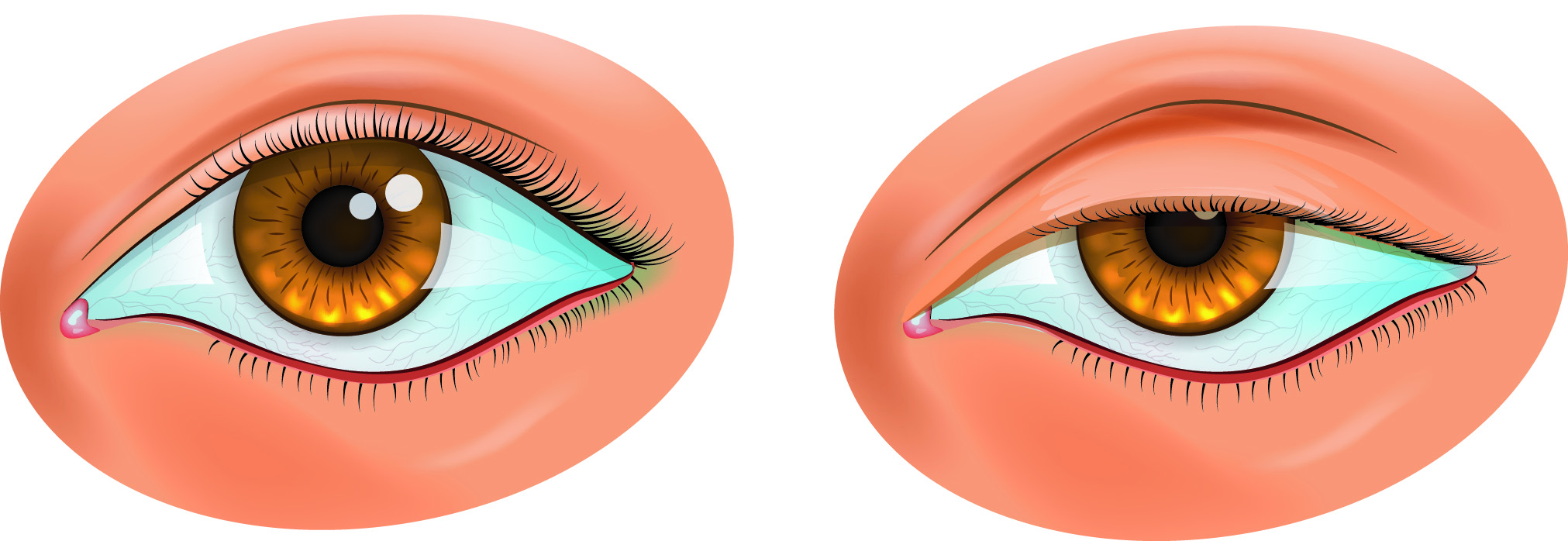
Ptosis is an abnormally low position of the upper eyelid. It is more common in older patients due to a gradual loss of function of the muscles working to hold the eyelids up. However, it can be due to other, more serious reasons.
Types of Ptosis
That pesky drooping lid can be classified broadly based on the cause. Myogenic ptosis means a weak muscle function, while aponeurotic ptosis means the muscle works but is stretched out. Mechanical ptosis is when there is something physically pushing or weighing down the lid. Traumatic ptosis is based on a history of trauma. Pseudoptosis means it’s not the lid itself drooping, but another anatomical anomaly can make it look this way. For example, the other eyelid could actually be contracted, making the lid appear low comparatively. Neurogenic means there is some sort of problem with the nerve controlling the eyelid function. This is the ptroublesome one that makes us sweat a little bit. What should you do next?
Rule Out the scary stuff
- Cranial Nerve III Palsy
Ask your patient: Was this noticed suddenly? Are you experiencing double vision? Do you have any systemic diseases that can affect blood supply such as diabetes or hypertension?
Look for: The affected eye is pointed down and out. The pupil is dilated*. - Horner syndrome
Ask your patient: Is there a loss of ability to sweat on this area of your face? Any head or neck trauma? Any surgery to your heart, thyroid, or neck?
Look for: A small pupil that lags to dilate*. - Myasthenia Gravis
Ask your patient: Is the drooping worse at the end of the day? Do you have limb weakness during any daily activities such as walking up the stairs? Difficulty breathing*?
Look for: Eyelid muscles are weak and gets tired very quickly. - Malignancy
Ask your patient: Was this a sudden onset?
Look for: Exophthalmos. Pupil involvement*
*You will be referring these patients for imaging urgently. Pupil involvement or trouble breathing can be signs of further or more complicated problems.
You’ve taken the appropriate history. What’s next?
Further testing
- Pupil size & function, along with extraocular motility:
While you are going to do this on every patient, it’s important to observe carefully for ptotic patients. This is to rule out a neurological cause of ptosis. - Marginal reflex distance (MRD):
This actually entails two measurements. Ask the patient to view a distance target, hold a penlight centrally about 40cm away & use your pocket ruler to measure. MRD-1 is the distance between the pupillary reflex and the upper lid margin. The typical range is 4-5mm. MRD-2 is the distance between the pupillary reflex and the lower lid margin. This is usually slightly larger than MRD-1, approximately 5mm. - Levator function:
The levator palpebral superioris muscle lifts that eyelid, so check out how well it’s working. To do this, place your thumb above the eyebrow to make sure the frontalis muscle is not helping out. Ask the patient to look down and use the location of the upper lid margin as your zero point. Then ask the patient to look upward as far as they can & measure how far that upper lid has raised. - Fatiguability:
Ask the patient to look up continuously for 1 minute. Measure the height of the upper lid margin before & after. - Lid crease height:
With the patient looking down, measure the distance from their upper lid margin to the crease. There is natural variability in eyelid anatomy, but 6-10 mm is the average range for this. - Some not-so-stealthy snooping:
Ask to see an old photo (a driver’s license, health card, or old photo on their phone). Was the ptosis present before? Was it in the same eye? Was it better or worse in this photo compared to now?
The last word of advice for dealing with ptosis: Record record, record! Just like with anything else, proper recording is key. There’s a reason that a cliché in healthcare is “if you didn’t record it, it didn’t happen.” OK, now breathe a sigh of relief. Hopefully, these steps make you dread that darn droop a little bit less.
References:
(2008). Chapter 6. In J. P. Ehlers & C. P. Shah (Eds.). The Wills eye manual: office and emergency room diagnosis and treatment of eye disease (p128-130). Philadelphia: Lippincott, Williams & Wilkins.
Wesley Klejch, BS., Vilisel, JM., & Allen, RC. (April 2015). A Primer on Ptosis. University of Iowa Health Care, EyeRounds.org. Retrieved from http://webeye.ophth.uiowa.edu/eyeforum/tutorials/ptosis/index.htm
Sreekanth, G. (Janu 2016). Ptosis Examination Dr. Gayathri Sreekanth. Retrieved from https://www.youtube.com/watch?v=v7v2GqXXk-8