Dear Diary,
Fourth year clinical rotations are the pinnacle of optometry school that all students are anxious for. It’s a time of freedom, learning, and exposure to parts of optometry you may never see in the school clinic. Or is it?
My name is Lawrence Yu, and I just started my clinical rotations as a fourth year student at the Southern California College of Optometry at Marshall B. Ketchum University. Through this blog, I will chronicle and share my rotations experience throughout the year at my four different sites. Join me as I leave the safety of the school clinic and enter the real world of optometry. Learn with me as I see some crazy eye diseases. Suffer with me as I endure moving every 2.5 months. Follow me and prepare yourself for your last year of optometry school.
—
Thursday, June 12, 2014
Refractive Surgery: Day 18 of 79 at Naval Medical Center of San Diego
Everybody wants refractive surgery. 75% of the patients I have seen at my first rotation site have casually asked me, “So can I get that surgery to fix my vision?” To handle this increasing demand, it’s to our benefit as optometrists to understand refractive surgery. What better way to learn than to watch?
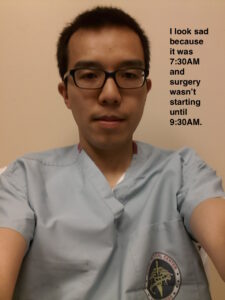
In the morning, I went to the refractive surgery center and was directed to put on scrubs before sitting in on live refractive surgeries. I had never put on scrubs before, so I put it on over my dress shirt. After realizing how dumb I looked with my sleeves sticking out, I properly took off my dress shirt before putting on the top. I then had to tie a facemask and hairnet on, and that was a mess because of all the loose strings flying around. The ophthalmologist had to help me tie it all up – co-management at its finest.
That morning I observed five LASIK operations and three PRK operations. Each surgery was extremely quick and efficient, and I was reminded of a pit stop at a car race. Each technician knew exactly what he or she had to do at precise times in the surgery. Two technicians revolved around the ophthalmologist as he operated the femtosecond laser to cut the corneal flap and then the excimer laser to ablate the cornea. Each surgery took about 10-15 minutes, and the procedure was highly repeatable. Watching the surgery was just like watching the LASIK videos on YouTube, but now I could see the great speed, efficiency, and logistical handling of how ophthalmologists conducted refractive surgery.
 The next day I saw the same patients at 1-day post-op appointments with the optometrists. Many of them were doing fine and had great vision. Similarly to watching the surgery, there was technically not much to see, but I absorbed the proper ways to educate patients on post-surgical symptoms and potential problems. Although the ophthalmologist did the surgery, the optometrist was the one to manage patient expectations and questions about halos, glare, or dry eye. I picked up on the proper ways of describing the healing process in common terminology to patients. By providing timelines of expected post-surgical symptoms, the optometrist instilled ease into many of the patients.
The next day I saw the same patients at 1-day post-op appointments with the optometrists. Many of them were doing fine and had great vision. Similarly to watching the surgery, there was technically not much to see, but I absorbed the proper ways to educate patients on post-surgical symptoms and potential problems. Although the ophthalmologist did the surgery, the optometrist was the one to manage patient expectations and questions about halos, glare, or dry eye. I picked up on the proper ways of describing the healing process in common terminology to patients. By providing timelines of expected post-surgical symptoms, the optometrist instilled ease into many of the patients.
In the next blog entry, I’ll talk about some of the tests the optometrists did to evaluate if a patient was a good refractive surgery candidate. I greatly underestimated the amount of technology used.
Some miscellaneous tips I learned in my time at the refractive surgery center:
– DLK is best seen with retroillumination on slit lamp. They are so fine that direct white light would bleach them out of view.
– In PRK, the cornea is healing and may actually induce a ton of astigmatism on the way. If you check back in a few weeks when healing is complete, that temporary astigmatism can disappear.
– Meibomian gland secretions can get under the corneal flap and look very similar to inflammatory white blood cells. The secretions can be of any size while cells would all look the same size.