Background: Both a pinguecula and a pterygium are forms of conjunctival elastic degenerations of the stroma that are caused by chronic exposure to sunlight, wind, and dry eye conditions. They are seen in individuals who do regular work outdoors. To a student just learning ocular disease, these two conditions may be confused for one another. While these two conditions share the similarity of being a degeneration of the bulbar conjunctiva, there are distinct differences. This article aims to outline the two conditions and provide a picture of each, for comparison.2
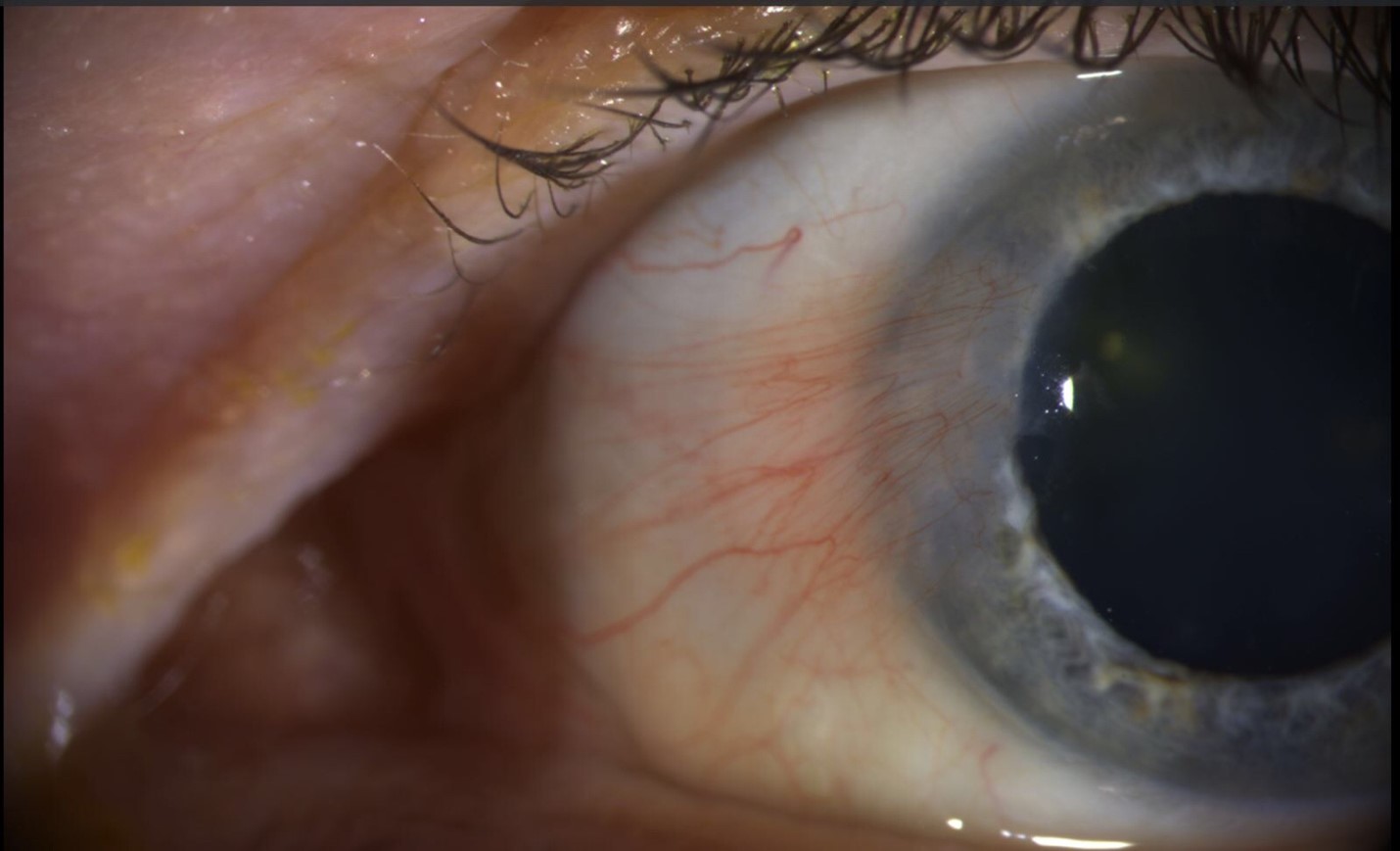
PINGUECULA
Pathophysiology and Appearance: A pinguecula (plural pingueculae) is a highly common, benign, asymptomatic, elastotic degeneration of the conjunctival stroma. This condition is characterized as a yellow-white mound or cluster of mounds seen on the bulbar conjunctiva adjacent to the limbus. It is seen at both the nasal and temporal limbus, but it is more frequently seen at the nasal location. Additionally, the limbus serves as a barrier, as the pinguecula will extend from the bulbar conjunctiva to the limbus, but not encroaching on the cornea. Calcification can be present if actinic damage is suspected. Occasionally, a pinguecula can become acutely inflamed, known as pingueculitis, if the lesion is large or has overlying calcification that cause epithelial breakdown.2
 Treatment: Treatment is usually unnecessary due to the slow growth of the lesion.
Treatment: Treatment is usually unnecessary due to the slow growth of the lesion.
- All cases: Patients are advised to wear sunglasses to reduce ultraviolet exposure from the sun and decrease the progression. Protection against dust and wind is also recommended.
- Mild cases: Occasional irritation and dryness can be relieved with topical lubrication, such as preservative-free artificial tears.
- Moderate Cases & Pingueculitis: Mild to moderate forms of pingueculitis can be treated with topical lubrication in addition to a short course of topical steroid can be added to the treatment of pingueculitis is the patient has marked irritation. A soft steroid, such as Loteprednol QID for 7 days, can be used as part of this steroid treatment.
- Severe cases: If significant irritation persist, excision can be performed. A pinguecula can also be excised for cosmetic reasons. Recurrence rate is very low, so simple excision of the lesion is very successful. Thermal laser ablation can also be effective, and gentian violet markings may be required in lighter-skinned individuals to ensure adequate absorption.2
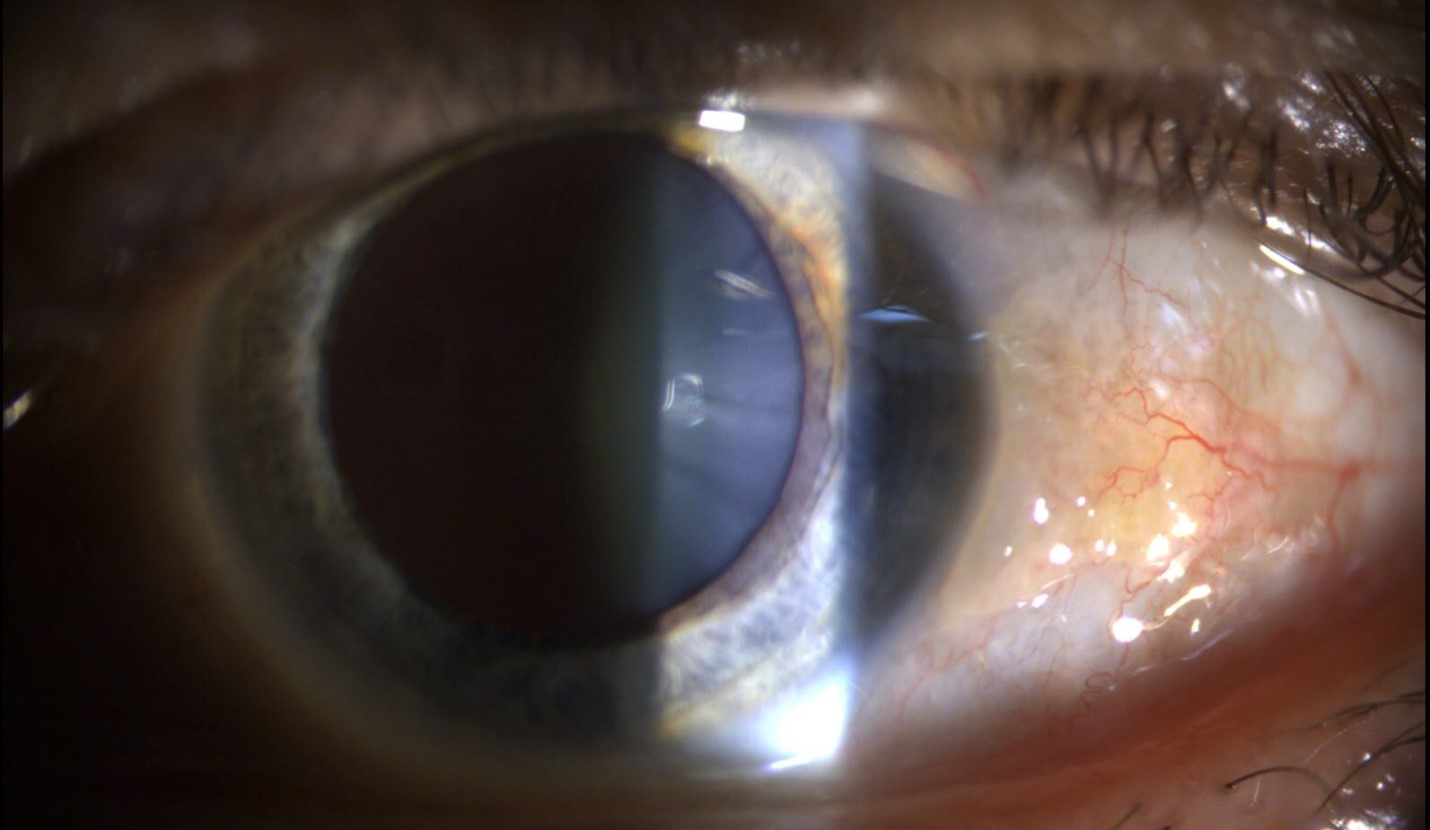
PTERYGIUM
Pathophysiology and Appearance: A pterygium (pleural pterygia) is a triangular-shaped, fibrovascular, subepithelial in-growth due to the degeneration of the bulbar conjunctiva. The apex of pterygium points toward the cornea. This degeneration occurs over the limbus and encroaches onto the cornea. It typically is seen in patients who live in hot climates and have been exposed to ultraviolet exposure, wind, and chromic eye dryness. A pterygium shows elastotic degeneration in vascularized, subepithelial stroma collagen. Pterygia encroach onto the cornea at the level of Bowman’s layer. Additionally, WTR astigmatism can me induced due to the flattening of the horizontal meridian. A Stocker line, or a linear epithelial iron deposit, can be seen within the corneal epithelium. Pseudo-pterygia have a similar appearance to a pterygium; however, a pseudo-pterygium is caused by a band of conjunctiva adhering to an area of compromised cornea at the level of the apex. These “false pterygia” occur in response to an acute inflammatory episode (chemical burn, corneal ulcer, trauma, or cicatrizing conjunctivitis).2
 Symptoms: Most small lesions are asymptomatic. Grittiness and irritation are typically caused by a dellen (localized drying) at the advancing edge due to interference with the pre-corneal tear film. Patients who wear contact lenses may notice irritation earlier than in non-contact lens wearers due to the edge lift. Additionally, lesions may interfere with vision by inducing astigmatism or in reaching into the line of sight. Intermittent inflammation, additionally, may also occur.2
Symptoms: Most small lesions are asymptomatic. Grittiness and irritation are typically caused by a dellen (localized drying) at the advancing edge due to interference with the pre-corneal tear film. Patients who wear contact lenses may notice irritation earlier than in non-contact lens wearers due to the edge lift. Additionally, lesions may interfere with vision by inducing astigmatism or in reaching into the line of sight. Intermittent inflammation, additionally, may also occur.2
Treatment:
- All cases: Patients are advised to wear sunglasses to reduce ultraviolet exposure from the sun and decrease the progression. Protection against dust and wind is also recommended. A lubricating drop to relieve dryness.
- Mild cases: An artificial tear can be used in mild cases four times a day, or the preservative free drops can be used eight times a day with more advanced dryness.
- Moderate-severe cases: For moderate and severe conditions, a mild topical steroid (fluorometholone ophthalmic suspension 0.1% QID), a non-steroidal, anti-inflammatory drop (ketorolac 0.4% to 0.5%), or a topical antihistamine + mast cell stabilizer (bepotastine, ketotifen, olopatadine) may be used to decrease symptoms. If a dellen occurs, an artificial tear ointment can be used q2h.
- Severe cases: Surgical incision is indicated in the following conditions: the pterygium extends into the visual axis or induces significant astigmatism, the patient experiences excessive irritation with no relief from conservative treatments, or the lesion interferes with contact lens wear. Simple excision is associated with an 80% chance of recurrence. The bare sclera dissection with a conjunctival autograft or amniotic membrane graft helps to reduce the recurrence rate. Intraoperative applications of mitomycin C can also help reduce occurrence. Antimetabolites are typically used for excision of recurrent pterygia due to these medications having an increased risk of corneoscleral thinning or necrosis. The recurrent pterygia tend to be more aggressive than the original pterygium. Peripheral lamellar keratoplasty may be indicated for deeper, penetrating lesions.1
Follow-Up: Patients without symptoms can be checked during annual exams. Pterygia are typically measured periodically initially to determine the rate of growth towards the visual axis. If treatment includes a topical steroid, an IOP check and anterior segment check needs to be performed within a few weeks to monitor IOP and inflammation, respectively. The non-steroidal drop can be used can be used periodically for a limited duration of time; the mast cell stabilizer + topical antihistamine can be used PRN.1
References:
- Bagheri, N., & Wajda, B. (2017). The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease (7th ed.). Philadelphia: Wolters Kluwer.
- Bowling, B., & Kanski, J. J. (2016). Kanski’s Clinical Ophthalmology: A Systematic Approach (8th ed.). Edinburgh: Elsevier.

